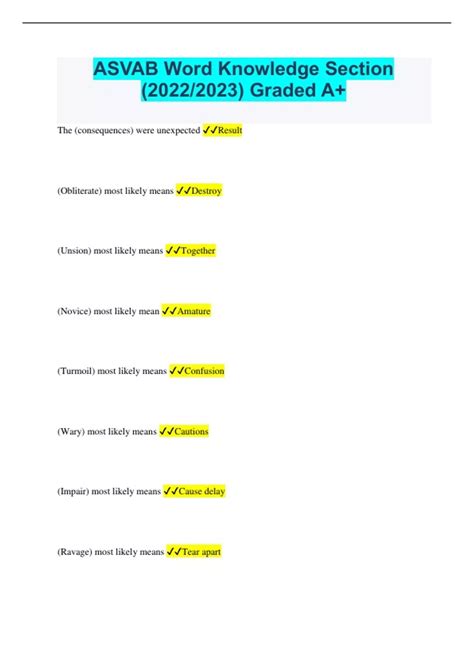
10+ Col11a1 Strategies: Your Complete Guide To Poag And Pacg
Understanding Col11a1: A Key Component in POAG and PACG
Col11a1, also known as collagen type XI alpha 1 chain, is a crucial protein that plays a significant role in the development and progression of two eye conditions: Primary Open-Angle Glaucoma (POAG) and Primary Angle-Closure Glaucoma (PACG). These conditions, if left untreated, can lead to vision loss and even blindness. In this comprehensive guide, we will explore the various strategies and treatments available to manage Col11a1-related eye disorders, providing you with the knowledge to take control of your eye health.
The Role of Col11a1 in Glaucoma
Col11a1 is a vital component of the extracellular matrix (ECM) in the eye, particularly in the vitreous humor and the trabecular meshwork. The vitreous humor is a gel-like substance that fills the back of the eye, while the trabecular meshwork is a complex network of cells and tissues responsible for regulating the outflow of aqueous humor, the fluid that maintains eye pressure.
In individuals with POAG and PACG, mutations or abnormalities in the Col11a1 gene can lead to structural changes in the ECM, affecting the drainage of aqueous humor and resulting in increased intraocular pressure (IOP). Elevated IOP is the primary risk factor for both types of glaucoma, as it can damage the optic nerve and cause irreversible vision loss.
Diagnosing Col11a1-Related Glaucoma
Accurate diagnosis is crucial for effective management of Col11a1-related glaucoma. Ophthalmologists use a combination of clinical examinations and diagnostic tests to identify these conditions:
- Tonometry: This test measures the pressure inside the eye, helping to detect elevated IOP.
- Ophthalmoscopy: By examining the back of the eye, including the optic nerve and retina, ophthalmologists can identify signs of damage caused by increased IOP.
- Gonioscopy: This procedure allows doctors to visualize the angle between the cornea and the iris, aiding in the diagnosis of PACG.
- Visual Field Testing: This test assesses the patient’s peripheral vision, which is often affected in glaucoma.
- Optical Coherence Tomography (OCT): OCT provides detailed images of the retina and optic nerve, helping to detect early signs of glaucoma.
- Genetic Testing: In some cases, genetic tests can identify mutations in the Col11a1 gene, confirming the diagnosis of Col11a1-related glaucoma.
Treatment Strategies for POAG and PACG
Managing Col11a1-related glaucoma requires a multi-faceted approach, and treatment options may vary depending on the severity of the condition and individual patient needs. Here are some common strategies:
Medications
- IOP-Lowering Eye Drops: These are the first-line treatment for glaucoma. They work by either reducing the production of aqueous humor or improving its outflow, thus lowering IOP.
- Oral Medications: In some cases, oral medications may be prescribed to further reduce IOP.
Laser Treatments
- Selective Laser Trabeculoplasty (SLT): SLT is a minimally invasive procedure that uses a laser to stimulate the trabecular meshwork, improving aqueous humor drainage.
- Laser Peripheral Iridotomy (LPI): LPI is commonly used in PACG to create a small hole in the iris, allowing fluid to flow more freely and preventing sudden angle-closure attacks.
Surgical Interventions
- Trabeculectomy: This surgical procedure creates a new drainage pathway for aqueous humor, bypassing the blocked or damaged trabecular meshwork.
- Glaucoma Drainage Devices (GDDs): GDDs, such as Ahmed glaucoma valves, are implanted to facilitate the drainage of aqueous humor and reduce IOP.
- MIGS (Minimally Invasive Glaucoma Surgery): MIGS procedures are less invasive than traditional surgeries and can be effective in lowering IOP.
Lifestyle Modifications and Support
In addition to medical treatments, certain lifestyle changes and support measures can help individuals with Col11a1-related glaucoma manage their condition:
- Regular Eye Exams: It is crucial for individuals with glaucoma to have regular eye exams to monitor their eye health and adjust treatments as needed.
- Healthy Lifestyle Choices: Maintaining a healthy weight, exercising regularly, and eating a balanced diet can positively impact eye health.
- Eye Protection: Protecting your eyes from injury is essential, as trauma can worsen glaucoma.
- Support Groups: Connecting with others who have glaucoma can provide emotional support and valuable insights into managing the condition.
Research and Future Prospects
Research into Col11a1 and its role in glaucoma is ongoing, offering hope for improved treatments and potentially even a cure. Some areas of focus include:
- Gene Therapy: Scientists are exploring the possibility of using gene therapy to correct Col11a1 mutations and prevent the development of glaucoma.
- Stem Cell Research: Stem cells may hold the key to regenerating damaged eye tissues, offering a potential cure for glaucoma.
- Pharmacogenomics: Understanding how genetic variations affect an individual’s response to glaucoma medications could lead to more personalized treatment plans.
Conclusion
Col11a1-related glaucoma, including POAG and PACG, can be managed effectively with a combination of medical treatments, lifestyle modifications, and ongoing research. Early diagnosis and consistent management are crucial for preserving vision and preventing further damage. By staying informed and proactive, individuals with these conditions can take control of their eye health and maintain a high quality of life.
FAQ
What are the early signs of POAG and PACG?
+Early signs of POAG and PACG can be subtle and often go unnoticed. However, some common symptoms include gradual peripheral vision loss, difficulty adjusting to dark environments, and the appearance of halos or rings around lights. Regular eye exams are crucial for early detection.
Can lifestyle changes alone manage glaucoma?
+While lifestyle changes can positively impact eye health, they are not a substitute for medical treatment. However, adopting a healthy lifestyle can complement medical interventions and potentially slow the progression of glaucoma.
Are there any natural remedies for glaucoma?
+Currently, there is no scientific evidence to support the use of natural remedies as a primary treatment for glaucoma. However, certain supplements like omega-3 fatty acids and antioxidants may have potential benefits for eye health. Always consult with your doctor before trying any natural remedies.
How often should I have eye exams if I have glaucoma?
+The frequency of eye exams depends on the severity of your glaucoma and your individual needs. Typically, individuals with glaucoma should have eye exams every 3-6 months to monitor their eye health and adjust treatments as necessary.
What are the potential risks of laser treatments for glaucoma?
+Laser treatments for glaucoma are generally safe and effective, but like any medical procedure, there are potential risks. These may include temporary inflammation, increased IOP, and, in rare cases, damage to the cornea. Your ophthalmologist will discuss these risks with you before the procedure.